Biobanking is a way of storing biological samples from women who have had breast cancer, and is a valuable resource for new discoveries. There are several biobanks in Australia, including the Monash University Biobanking Victoria Facility. This biobank, launched in 2020, contains 4.5 million biological samples and is already supporting six clinical trials.
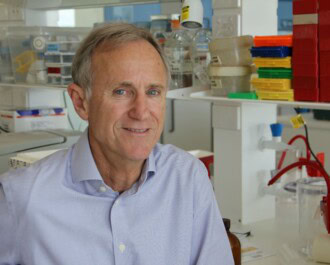
Biobanking Victoria supports a study led by NBCF-funded researcher Professor Melissa Southey. Prof Southey is the Director of the Biobanking Victoria Initiative, Chair of Precision Medicine and Distinguished Professor in the School of Clinical Sciences at Monash Health, Monash University.
In this study, resources provided by 30,000 women dating back to the mid 1990s were re-examined using new knowledge and techniques. The researchers completed targeted-sequencing of 24 genes that were potentially linked with breast cancer susceptibility, in samples from women with breast cancer, those without, and family members from both groups.
In one in 20 of the breast cancer cases, Prof Southey’s team found new genetic mutations that were not identified when the women were originally diagnosed and underwent genetic testing. They were then able to communicate the new findings to the women, providing them with answers many had been seeking for decades.
The study found that about 1.5% of the women retested, who did not have mutations in BRCA1 or BRCA2, had a mutation in another gene called PALB2. Women who have a mutation in PALB2 have about a 53% chance of developing breast cancer by age 80, about four times the risk of a non-carrier.
The results of this study, and previous work by Prof Southey’s team, have led to changes in the eviQ cancer genetics clinical guidelines that now include support for routine genetic testing and cancer risk management for PALB2 mutation carriers, in addition to standard BRCA1 and BRCA2 tests. These guidelines are an online resource that health professionals can access for the latest information on best practice cancer genetics information.
Prof Southey said that the advances in technology, and the increased number of known genes in which mutations increase the risk of breast cancer, meant that answers could now be found for many more women and their families.
“We now have a number of other genes (apart from the well-known BRCA1 and BRCA2) that we can test for with new technology, that provides really helpful information about the cancer risk a person faces now and, in the future,” she said.
Dr Tu Nguyen-Dumont, an NBCF-funded Career Development Fellow and the Head of the Clinical Genomics Laboratory in Precision Medicine at Monash University said this work enables predictive testing (or testing of family members), that further increases the opportunities for early detection and prevention before cancer arises.
“Most people who received new genetic information via the conduct of this study were really pleased to hear that there was an explanation for their cancer predisposition, and it now gives them an opportunity to be much more informed and proactive about cancer prevention strategies.”
More News Articles
View all News