
BREAST CANCER TREATMENT
This article includes a summary of various breast cancer treatments available and what to expect with each treatment option. See the contents below to jump to the section most relevant to you.
Type of Breast Cancer Treatment
There are a number of breast cancer treatment options in Australia. The choice of treatment depends on a number of factors, including:
- The type of breast cancer
- The location of tumour in the breast
- The tumour’s stage and grade
- Molecular characteristics of the tumour (hormone receptor status)
- The age, health and preferences of the patient
- Whether the patient had breast cancer before and what treatments have been used
One or more treatments may be recommended, and treatments may be provided in different sequences and combinations.
Common types of breast cancer treatment options are described below. These descriptions are not intended to be exhaustive or replace professional medical advice. Please consult with your doctor or cancer care team if you are concerned about the risks and side effects of any recommended treatment.
Surgery
Surgical treatment is an operation where the doctor removes the tumour. This is one of the most common treatment options for women with breast cancer. The two main types of surgery are breast-conserving surgery and mastectomy. For more information on surgery click here.
-
Lumpectomy
Also known as lumpectomy or wide local excision. The surgeon removes the tumour and some surrounding healthy tissue, leaving as much breast tissue as possible.

“This photo was taken the night post my lumpectomy. I remember feeling an overwhelming sense of relief that the cancer was finally out. Two weeks later, I received the news that I had a complete pathological response to chemotherapy and immunotherapy. None of this would have been possible if it wasn’t for all the research that has gone into this disease.” Ana, diagnosed 2018
-
A mastectomy
Is the removal of the entire breast. Some women may choose to have a double mastectomy, where both breasts are removed. A woman may opt to have breast reconstruction surgery at the same time as her mastectomy, but it may also occur later as a separate operation. For more information on a mastectomy, click here.
Chemotherapy
Chemotherapy (often referred to as ‘chemo’) is the administration of anti-cancer drugs to kill cancer cells.
Chemotherapy can be given intravenously (injected into your vein) or orally. The drugs used will depend on the type and stage of breast cancer. There are often side-effects associated with chemotherapy, including nausea, fatigue, hair loss, mouth ulcers and constipation.
- Neoadjuvant chemotherapy
In some cases, chemotherapy may be recommended before surgery (called neoadjuvant chemotherapy) as it may shrink the tumour and provide the patient with more surgical options. - Adjuvant chemotherapy
When chemotherapy occurs following surgery, it is referred to as adjuvant chemotherapy. Adjuvant chemotherapy may be used to kill any cancer cells that remain or to lower the risk of cancer recurrence.
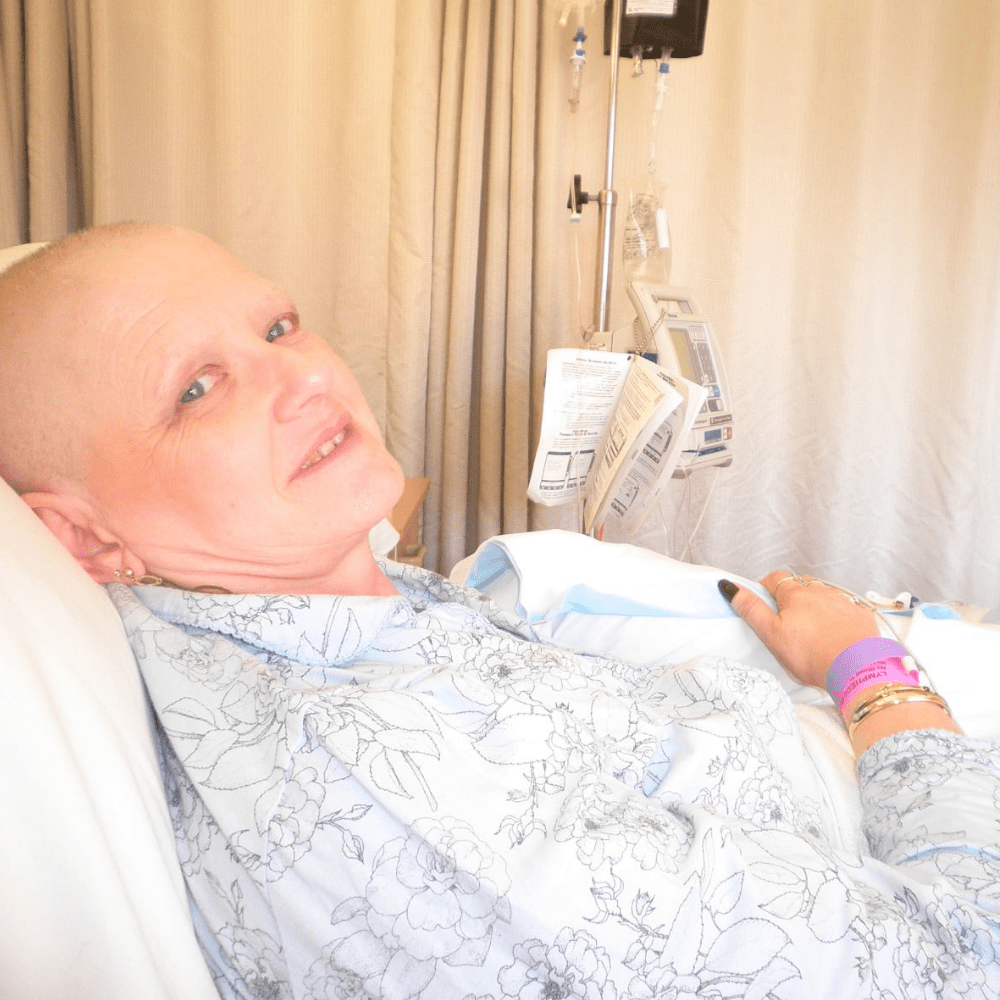
“This photo was taken on my seventh lot of chemo. I have been having chemo for 10 years now one way or another. Thank you to NBCF funded researchers who are looking at ways to prevent, detect, monitor, and treat breast cancer to ultimately save lives. We know that 9 Australians die each year from breast cancer which is really sad and my family thinks about this every day with me as I have advanced breast cancer but I want to say a huge THANK YOU to the doctors and researchers who are trying to keep me alive.” Tracey, diagnosed 2010

“This is the night I decided to shave my head just before my second chemotherapy. I was losing it in handfuls and the pain was indescribable. This was my chance to take control of one thing throughout this cancer journey. I actually felt very empowered taking this photo!” Natalie, diagnosed 2018
Radiotherapy
Radiotherapy (also called radiation therapy) is the use of targeted radiation, such as x-rays, to destroy cancer cells or keep them from growing.
Radiotherapy may be given externally or internally.
- External radiation therapy uses a machine outside the body to irradiate the cancer.
- Internal radiation therapy uses a radioactive source put inside the body for a short period of time. The source is placed directly into or near the cancer.
Radiotherapy may have side-effects such as fatigue, skin changes in the treatment area (such as redness or skin peeling) and swelling of the breast.
 “This is a photo of my third active stage of treatment – radiotherapy. My treatment plan was tailored to my specific type of breast cancer, such precision medicine wouldn’t be possible without research.”
“This is a photo of my third active stage of treatment – radiotherapy. My treatment plan was tailored to my specific type of breast cancer, such precision medicine wouldn’t be possible without research.”
Sarah, diagnosed 2021
Hormone therapy
Hormone therapy (also called endocrine therapy or hormone-blocking therapy) is used to treat hormone receptor positive breast cancers (cancers with oestrogen and/or progesterone receptor) that likely require hormones to grow.
Hormone therapy can be given orally (such as the medication Tamoxifen), or through injections (such as the drug Fulvestrant, which may be used to treat metastatic breast cancer).
Side effects may include menstrual changes, hot flushes, and night sweats; Tamoxifen can also increase the risk of blood clots, although blood clots are rare.
Targeted therapy
Targeted therapy is a type of cancer treatment that works differently to chemotherapy. Chemotherapy attacks all rapidly dividing cells in the body, but targeted therapy works by “targeting” those differences that help a cancer cell to survive and grow.
Targeted treatments can be taken orally, injected or given intravenously (through a vein). They may be given along with chemotherapy.
Side effects of targeted therapy can include fever, headache, and a rash; the targeted therapy trastuzumab (brand name Herceptin) may also affect heart function.
Treatment for advanced and metastatic breast cancer
Advanced breast cancer (also referred to as metastatic breast cancer) occurs when breast cancer has spread (or metastasised) to other parts of the body. Treatment of metastatic breast cancer aims to control the growth and spread of the cancer, to relieve symptoms, reduce pain, and improve or maintain quality of life.
Treatment options can include surgery, radiation, chemotherapy, hormonal therapy and/or targeted therapy, depending on the location and molecular makeup of the cancer. Treatment may shrink or slow the growth of tumours, ease symptoms and help women live longer.
New breast cancer treatments
With the help of scientific research, a number of new treatment options are currently being developed to improve treatment effectiveness and reduce potential side effects. These include new approaches to treat advanced breast cancer, harnessing the patient’s immune system to fight cancer (immunotherapy) and personalising cancer treatment. Learn more about these different treatment approaches and the related NBCF research projects below.
Immunotherapy in breast cancer
Immunotherapy is a type of cancer treatment that uses the body’s immune system to fight against cancer. Immunotherapy may slow the growth and spread of cancer by helping the immune system destroy existing cancer cells. Rarely, immunotherapies may also cause other severe, potentially life-threatening reactions.
In Australia, immunotherapies have been approved for some cancers (such as melanoma and lung cancer) but not yet for breast cancer. However, immunotherapies are currently being tested in clinical trials (research studies where people volunteer to test new treatments) for breast cancer in Australia. This includes two groundbreaking clinical trials (called CHARIOT and DIAmOND) from NBCF-funded researcher and Endowed Chair, Professor Sherene Loi. These trials will hopefully lead to regulatory approval and ultimately, impact the future of breast cancer treatment.
Towards personalised medicine
Personalised medicine (also referred to as precision medicine) refers to a treatment approach where cancer treatment is tailored to an individual patient, using information such as the tumour’s molecular makeup, size, and spread, as well as the patient’s genes. The goal is for doctors to make optimal treatment choices to maximise effectiveness and avoid side effects, using a customised rather than ‘one-size-fits-all’ treatment approach, leading to fewer deaths and better quality of life for those diagnosed.
However, the success of personalised medicine depends on being able to identify the right treatment for the right person at the right time. This is a great challenge, as breast cancers can vary genetically and biologically from one another; even the same cancer can change over time within the same patient. Therefore, there is an urgent need to identify biological features (or ‘biomarkers’) that can distinguish different patient groups from one another and predict their response to treatment.
Hear from Professor Alexander Swarbrick on research into personalised treatment options
Cost of breast cancer treatments
Breast cancer patients may access medicines or medical services via a range of ways:
1) The Pharmaceutical Benefits Scheme (PBS). If medicines or medical services are approved by the PBS then they are provided to patients at a Government subsidised price.
2) Private health insurance. Patients should contact their insurer for information whether prescribed medicines and medical services are covered by their insurer.
3) Compassionate/special access programs. In some circumstances. pharmaceutical companies may provide patients with discounted or free access to new medicines not yet approved by the PBS.
4) Clinical trials. Depending on eligibility, patients may gain early access to new medicines that have not yet received Therapeutics Goods Administration (TGA) approval or PBS listing. Clinical trials may be sponsored by pharmaceutical companies or initiated by researchers and health professionals.
5) Out of Pocket. In some cases, medicines and services that are not available by any of the above means may require out of pocket costs.
All the potential options for accessing breast cancer treatments should be discussed with your medical oncologist. Please visit here if you require any further information.