Dozens of Victorian women affected by the most common breast cancer will be first in the world to try a new treatment mix that aims to switch off tumour cells’ ‘survival factor’.
Researchers at the Walter and Eliza Hall Institute of Medical Research grew tumours, using samples from women who had had breast surgery, and then used them to test the therapy’s effectiveness.
The exploratory treatment combines the hormone therapy Tamoxifen with an anti-cancer compound. Known as BH3-mimetics, it works by binding to and neutralising the effects of a family of proteins called BCL-2, which keeps cancer cells alive.
This is a new class of cancer treatment which is also being tested in treating chronic lymphocytic leukaemia.
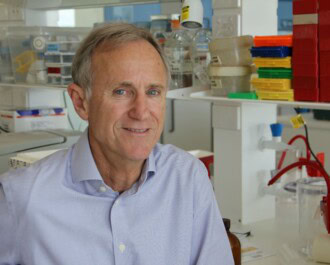
The head of the Institute’s breast cancer laboratory, Professor Geoff Lindeman, who was recently elected a Fellow of the Australian Academy of Science, said that in preclinical tests the new combination therapy delayed the growth of tumours or made them disappear.
The first of 24 patients will begin receiving the new combination therapy next month.
“Chemotherapy and hormone therapy can work very effectively to kill cancer cells, but if you have high levels of a survival factor, it makes it much more difficult for these drugs to do their work,” said Prof Lindeman. “We know from our preclinical work that single agent therapy doesn’t appear to be effective.
“We almost have to hit the cells with another insult. That makes them more vulnerable for targeting cell death,” said Prof Lindeman, who is funded by the National Breast Cancer Foundation (NBCF), and also serves on the Foundation’s Research Advisory Committee.
Hormone-receptor positive breast cancer, also known as ER-positive, accounts for about 80 per cent of cases. In this cancer, the BCL-2 molecule is expressed in up to 85 per cent of cases.
The Institute’s team has just finished its phase I safety study to determine an effective dosage. The first of 24 patients, who have already had standard treatment, will begin receiving the new combination therapy from next month, at the Royal Melbourne Hospital.
Prof Lindeman says that if the combination treatment worked, the Institute plans to expand the trial to other hospitals around the country. This would include its use as a first line treatment.
“It’s an exploratory study,” Prof Lindeman said. “The goal is to improve the current strategy. It’s a big ask to cure cancer that has already spread and has become metastatic in the body. But to improve the response with a better quality and length of life, that’s certainly what we’re aiming for.”
Professor Lindeman’s research is funded by an NBCF novel therapy grant, and he says it’s always challenging to obtain funds for research. “NBCF has played a very important role contributing to our group’s research efforts. Without this sort of support, it would have been very hard for us to carry out our work in an internationally competitive manner,” he said.
More News Articles
View all News