Women with a gene mutation known to increase their cancer risk may have fewer eggs in their ovaries which may have implications for family planning, according to a study published overnight in the leading scientific journal Human Reproduction.
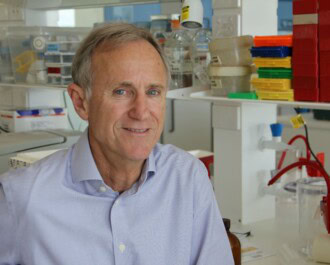
The international study led by Peter MacCallum Cancer Centre Oncologist and National Breast Cancer Foundation Fellow Professor Kelly-Anne Phillips checked the levels of anti-Müllerian hormone (AMH), which is an indicator of egg count, in women with either the BRCA1 or BRCA2 mutation.
Women with a BRCA2 mutation were found to have similar AMH levels to women of the same age who did not carry either mutation (non-carriers). However, women with a BRCA1 mutation had AMH concentrations that were, on average, 25 per cent lower than women of the same age who did not carry the mutation.
“This means that women in their mid-30s who carry the BRCA1 mutation have, on average, ovarian reserves similar to those of non-carriers who are two years older,” says Professor Phillips. Through a woman’s lifetime, AMH levels decline in line with the number of eggs remaining in her ovaries.
Professor Phillips says it was important to note AMH was only one indicator of potential fertility; women with low AMH levels can sometimes still have a baby while women with high AMH levels are sometimes unable to do so.
“However, our findings suggest that women carrying the BRCA1 mutation who wish to have children should avoid, where possible, delaying pregnancy until their late 30s or 40s when fertility is reduced anyway because of their age,” she says.
“For women trying to conceive in their 20s, any difference in ovarian reserve between BRCA1 mutation carriers and non-carriers is unlikely to be of clinical significance.”
The genetic mutations are rare in the general population – about 0.1 per cent of people have the BRCA1 mutation and around 0.2 per cent have the BRCA2 mutation – however prevalence is higher in certain groups such as Ashkenazi Jews. Women with these mutations are at higher risk of cancers of the breast, ovaries, fallopian tubes and peritoneum.
The study analysed AMH levels from almost 700 women, aged 25-45, and who were enrolled in kConFab (the Kathleen Cuningham Foundation Consortium for research into Familial Breast Cancer), a study supported by a grant from the National Breast Cancer Foundation. The researchers adjusted their analysis to take account of age, oral contraceptive use, body mass index and smoking.
In addition to BRCA1 mutations carriers having 25 per cent lower AMH concentrations, on average, than non-carriers, they were also more likely to have AMH concentrations that placed them in the lowest quarter when the women were divided into four groups according to the AMH levels. This was not seen in BRCA2 mutation carriers.
Inefficient DNA repair has been shown to contribute to the aging of a woman’s eggs and BRCA1 and BRCA2 are both integral to mending breaks that occur in DNA.
“BRCA2 has a more limited role in double-strand DNA break repair compared with BRCA1 and BRCA2 mutation carriers tend to develop fewer cancers and at a later age, compared with BRCA1 mutation carriers,” Professor Phillips says.
“So it is credible that any effect of mutation status on ovarian reserve would be more pronounced in BRCA1 mutation carriers. There may be a lesser effect in BRCA2 mutation carriers as well, but our study did not have adequate power to detect it.”
The study also suggests women with BRCA1 mutations who develop cancer could be at higher than average risk of early chemotherapy-induced menopause, though Professor Phillips says more research was needed to confirm this.
If you’d like to support breast cancer researchers like Professor Kelly-Anne Phillips, please donate.
More News Articles
View all News