Triple negative breast cancer (TNBC) is one of the most challenging to treat, as the tumours lack three receptors that are commonly targeted with therapy – oestrogen, progesterone and HER2. This means that people with TNBC have fewer treatment options and often a poor prognosis.
New research by a team from the Garvan Institute of Medical Research hopes to change this, after identifying four new cell types that are present in TNBC tumours. These cells may be targeted by drugs to slow the progression of the cancer, and offer new hope to patients.
Dr Sunny Wu, the first author of the study, explained “in our study, we searched for new potential targets for therapy by analysing the individual cells inside triple negative breast tumours. This includes not only the cancer cells themselves, but also the surrounding host cells, such as immune and connective tissue cells, which can be thought of as the cancer ‘ecosystem’ that supports a tumour to grow and spread.”
The team identified the cell types through genetic testing of over 24,000 individual cells in the tumours of five patients with TNBC. They detected over 6000 unique RNA molecules in every cell, which allowed them to create a profile of the cell’s gene activity. From this, four subtypes of stromal cells were identified. Stromal cells form the connective tissue of the body and, until now, it was thought that only one type existed in TNBC.
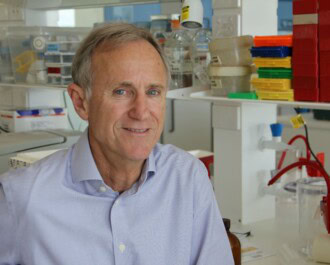
The study was led by NBCF-funded researcher Associate Professor Alex Swarbrick, who heads the Tumour Progression Laboratory at the Garvan Institute.
“Patients with triple negative breast cancers have a poor prognosis, in large part because treatment approaches have advanced very slowly,” says A/Prof Swarbrick. “We’ve analysed individual cells in patient tumour samples to gain unprecedented insights into what makes up a tumour, allowing us to identify subtypes of cells and investigate their role in disease.”

Associate Professor Alex Swarbrick.
One of the subtypes discovered, known as inflammatory cancer-associated fibroblasts or ‘iCAFs’, appear to suppress the body’s immune system, hence enabling increased tumour progression. It is hoped that by targeting the iCAFs with an additional treatment, the immune system will be able to fight cancer more effectively.
“Pathologists have been describing cancers under the microscope for more than 150 years, but we still only have a shallow understanding of the cells that are there,” says A/Prof Swarbrick.
“Cellular genomics is showing us that what we once thought of as one cell type is in reality a diversity of cell types, which will have a significant impact on how we tailor treatments in future.”
The study was supported by funding from the National Breast Cancer Foundation (NBCF) of Australia, Mr John McMurtrie AM and Mrs Deborah McMurtrie, G P Harris Foundation, Skipper-Jacobs Charitable Trust and the Sydney Breast Cancer Foundation, and published in the EMBO Journal.
“NBCF funded this project early in its development, at a time when it was considered high risk by other funding agencies. This investment by NBCF was essential to the success we see today, and we are very grateful for their ongoing support,” says A/Prof Swarbrick.
More News Articles
View all News