During April we saw research into potential vaccines for breast cancer, new genetic drivers, studies on treatment trends, and the good news that tamoxifen will be available as a preventative treatment for high-risk women.
New genetic drivers of breast cancer identified
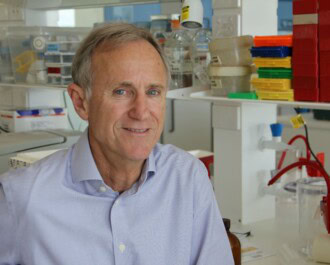
An NBCF-funded researcher at QIMR Berghofer Medical Research Institute in Queensland has co-led a major international study which has identified 26 genetic variants, or genetic ‘typos’, that increase a women’s risk of developing different subtypes of breast cancer.
Dr Stacey Edwards said that until now it wasn’t known if there was a genetic basis for ER-/PR-/HER2+ breast cancers, which make up a rare but treatable subtype of breast cancer. The findings will help doctors to predict those at a higher risk of developing breast cancer, and diagnose them more quickly so they receive the right treatment.
Research shows promise for breast cancer vaccine
The Mayo Clinic in the US will test two vaccines that could help the body fend off certain types of breast, ovarian and lung cancers. Researchers have been studying cancer vaccines for decades, with the aim of using the vaccine to teach the body’s immune system how to fight cancer.
Unlike traditional vaccines, which are used to prevent illnesses in healthy people, cancer vaccines in development are therapeutic, meaning they are used after a patient has been diagnosed with cancer – to prevent survivors from developing metastatic breast cancer.
NBCF note: NBCF-funded Dr Clare Slaney is developing an exciting new treatment which involves a transfusion of white blood cells plus the injection of a vaccine. The white blood cells are genetically modified to attack breast cancer cells, and the vaccine is made up of a virus that also has the power to attack cancer cells. She believes that once administered, the treatment could potentially remain effective even after the primary tumour is eradicated, eliminating any remnant or newly arising tumour cells. This is particularly important, as the threat of breast cancer recurrence in other organs is a constant worry for patients.
Cancer thwarts treatment by ‘stealing’ blood vessels
Cancers can resist treatment by ‘stealing’ blood vessels from nearby tissues, according to a new study which is the first to show that tumours can become resistant to drugs over time by learning to steal normal blood vessels from surrounding tissue – a process called vessel co-option.
The process of new blood vessel growth (angiogenesis) is important for cancers to grow, and several treatments have been developed to combat it, however, cancers often develop resistance to these treatments. Researchers found that cancer cells increase their ability to move when they co-opt vessels, and are looking into possible treatments to block co-option, angiogenesis and also cancer cell movement to successfully treat metastatic breast cancer.
NBCF funding leads to Australia’s first breast cancer prevention treatment listed on PBS
Thanks in part to funding from NBCF, tamoxifen is the first breast cancer prevention treatment to be added to the Australian Government’s Pharmaceutical Benefits Scheme. Now an estimated 250,000 women with a family history or a genetic predisposition to breast cancer can benefit from subsidised tamoxifen as a preventative measure.
Is breast conserving therapy or mastectomy better for early breast cancer?
Young women with early breast cancer face a difficult choice about whether to opt for a mastectomy or breast conserving therapy. New research has shown young women, who had early stage breast cancer that had not spread to the lymph nodes and who opted for breast conserving therapy with radiation therapy, had a 13% higher risk of developing a local recurrence of their disease over a 20-year period than women who had a mastectomy and no radiation therapy. Also, another US study has found that more women are opting for mastectomies, possibly unnecessarily.
NBCF note: Currently the majority of patients having breast conserving treatment undergo radiotherapy after surgery to reduce the risk of the cancer coming back in the breast. Recently MRIs have also been used to see if there is more than one cancer, which has led to more tissue being removed during surgery – however, it is not known if this actually helps women. Prof Bruce Mann was funded by NBCF to determine whether women can be safely treated without radiotherapy – possibly allowing many women to safely avoid both mastectomies and radiotherapy. We should know the outcome of this study in the near future.
More News Articles
View all News