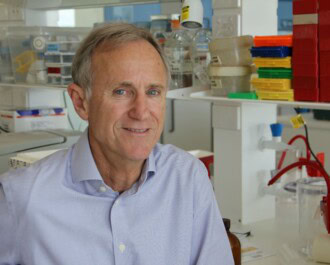
A team from the Harry Perkins Institute of Medical Research and The University of Western Australia, led by Associate Professor Pilar Blancafort, has discovered a new gene responsible for one of the most aggressive forms of breast cancer.
The gene, called AAMDC, is responsible for a subtype of hormone-sensitive breast cancer. Current treatment for this subtype is ineffective and leads to very aggressive disease, responsible for half of all breast cancer deaths.
Usually, hormone-sensitive tumours can be treated with medications that block the growth-promoting hormones, such as anti-estrogen therapies. However, there is a subgroup of women for whom the hormone therapies make things worse.
“A small percentage of patients experience a very aggressive cancer that results in the worst outcomes of all breast cancers, with half of all women dying from this subtype of disease,” said A/Prof Blancafort.
“When we look at these cancers, we find that they are bigger, tend to spread more commonly to the lymph nodes and have a higher death rate. What we needed was a way to identify them.”
To do this, the team accessed 119 breast cancer samples from a large study at Stanford University, and analysed the genetic profile of these tumours. They found that the most aggressive tumours had higher than normal levels of a cancer driving protein made by the AAMDC gene. This highly amplified gene that leads to the production of elevated levels of the AAMDC protein is found in about 10% of all breast cancers.
With the use of experimental models the team discovered that reducing the levels of AAMDC helped to slow down cancer progression. They also found that the AAMDC gene can help to protect tumours when they are starved of hormones, such as during anti-estrogen therapy.
“AAMDC can protect cancer cells from dying when the tumour is placed in conditions where nutrients are scarce and when it is starved of estrogen, which would kill most hormone-sensitive cancers,” A/Prof Blancafort explained.
“Therefore, we believe the cancer promoting function of AAMDC is to act as a ‘survival kit’, allowing tumors to adapt to these conditions, supporting the growth and multiplication of breast cancer cells in conditions of metabolic stress.”
This significant breakthrough means that scientists can now use the levels of AAMDC in a tumour to determine whether the patient is likely to respond well to hormone therapy. In addition, it opens a new avenue for treatments. It is possible that drugs that are already on the market may be able to be repurposed to block the action of this newly discovered breast cancer associated gene, hence improving outcomes.
The work was published in Nature Communications, and proudly supported by the National Breast Cancer Foundation through grants to A/Prof Blancafort and co-author Dr Anabel Sorolla.
More News Articles
View all News