Evidence-based clinical guidelines help physicians provide the best quality of care to their patients. In 2014, evidence-based guidelines for breast-conserving surgery, a common type of surgery used to remove breast cancer, was developed with the help of NBCF-funded researchers Dr Luke Marinovich (Curtin University) and Professor Nehmat Houssami (University of Sydney). These researchers have now led a study indicating that these guidelines have impacted clinical practice, helping to reduce unnecessary additional surgery in patients with breast cancer. The study was published in JAMA Surgery.
Breast-conserving surgery (or a lumpectomy) is one of two main types of surgery used to treat early stage breast cancer. During a lumpectomy, the surgeon aims to remove all of the tumour, plus a ring of normal tissue around the edges. This rim, called a surgical margin, is then examined by a specialist (pathologist) to ensure that it is clear of all cancer cells. During this examination, the pathologist will apply a special ink to the outer edges of the removed tissue so that its border is clearly visible under the microscope.
If cancer cells are present at the outer edge of the removed tissue, this is known as a positive margin. In such cases, additional surgery (re-operation) is usually needed to eliminate any remaining cancer cells. If no cancer cells are seen at the outer edge of the removed tissue, this is known as a negative margin (also referred to as a clear or clean margin), and no additional surgery is usually required.
Until 2014, there were no clear guidelines about what constituted a positive or negative margin. Hence, two leading professional organisations – the Society of Surgical Oncology (SSO) and the American Society for Radiation Oncology (ASTRO) – developed an evidence-based guideline that recommends “no ink on tumour” should be used to define a negative margin. Prior to the guidelines, less than 15% of surgeons accepted a margin of no ink on tumour for a lumpectomy. By standardising the definition, the SSO-ASTRO guideline sought to reduce unnecessary follow-up surgical procedures for patients, such as reoperations to obtain wider negative margins. More surgery usually means more discomfort and stress for the patient, and may lead to more complications.
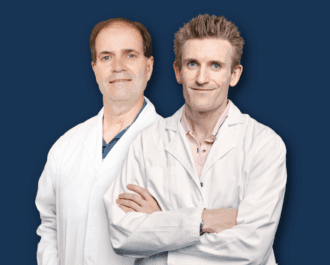
Dr Marinovich and Prof Houssami, who helped develop the 2014 guidelines, have now published a large systematic review showing that the guidelines have helped reduce unnecessary repeat surgeries worldwide. The review looked at almost 600,000 cases primarily from the US, UK and Canada, reported from 30 studies published between January 2014 to July 2019. The researchers found that the likelihood of having a reoperation after breast-conserving surgery was reduced after the publication of the SSO-ASTRO guideline.
While further work is needed to determine whether these changes are sustained in the longer term, the study indicates that the implementation of the guideline has improved clinical care in a relatively short time period.
“The findings suggest that the SSO-ASTRO guideline has had a positive impact on surgical practice for the treatment of early stage invasive breast cancer, playing a substantial role in reducing unnecessary surgery in patients with breast cancer,” said Dr Luke Marinovich, lead author of the study.
NBCF is proud to support these leading researchers through an Investigator grant to Dr Marinovich, and a Breast Cancer Research Leadership Fellowship to Professor Houssami.
More News Articles
View all News