Women with BRCA1 gene abnormalities have an increased risk of breast cancer if they have used hormonal contraception for at least one year.
New NBCF-funded research led by researchers at the Peter MacCallum Cancer Centre and Cancer Council Victoria links breast cancer risk with the use of hormonal contraceptives. These findings may impact the approach to decision-making about all aspects of patient care for BRCA1 gene abnormality carriers.
The research included almost 5,400 women who used hormonal contraceptives including the mini or combined contraceptive pill, hormonal implants or injections, or hormone-containing intrauterine devices (IUDs). The participants did not have cancer when they joined one of the long-term studies that were based in Australia, Europe, Canada or the United States between 1991 and 2019.
There were 3,882 women in the study with BRCA1 gene abnormalities and significantly, 488 of these later developed breast cancer.
Women who carry abnormalities in the genes BRCA1 and BRCA2 have a very high risk of developing breast cancer and this new research shows that the use of oral contraceptives adds to that risk for those with BRCA1 gene abnormalities, and for those who have used oral contraceptives for at least one year; with a proportional increase of risk of 3% per year of use.
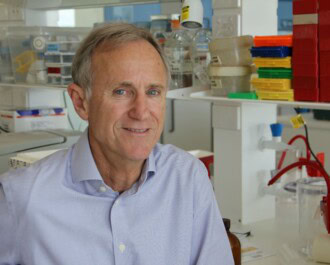
NBCF-funded researcher and principal investigator, Professor Kelly-Anne Phillips is a Consultant Medical Oncologist and Senior Strategic Research Leader at the Peter MacCallum Cancer Centre. Through her research, and over many years she has made significant progress in understanding how best to manage and care for those with a strong family history of breast cancer and who may carry BRCA1 and/or BRCA2 gene abnormalities.
Professor Phillips explains that despite the clear outcome of the study that shows an increased risk for developing breast cancer in women who carry BRCA1 gene abnormalities, “It doesn’t mean that we should tell all of these women not to use hormonal contraception.” Hormonal contraception is a very important health care option for women and carries both risks and benefits for all women. She suggests that instead, “It means that we really need to have personalised conversations with women about their own situation and to weigh up their individual absolute risk estimate with the other benefits of hormonal contraceptives.”
In this study, the relative risk associated with developing breast cancer varied according to how long hormonal contraceptives were used for and is just one of the factors that could affect an individual’s risk. More research is needed to understand how the use of hormonal contraceptives affects the risk of breast cancer in those who carry abnormalities in BRCA1, and if the risk of developing breast cancer differs between the use of specific hormonal contraceptive types such as hormonal IUDs, the contraceptive pill and hormonal implants.
This important research is just one example of how NBCF is funding world-class breast cancer research towards our vision of Zero Deaths from breast cancer. Empowering women with information and understanding about their cancer risk means that they can be effective advocates for their health. Together with their health professionals, they can actively participate in the decision-making process about their care to achieve the best possible outcome.
More News Articles
View all News