Breast cancer prevention and risk
Breast cancer is the most commonly diagnosed cancer amongst women in Australia. It is estimated that 1 in 7 women will be diagnosed with breast cancer in their lifetime.
However, anyone can be diagnosed with breast cancer. Around one in 600 men in Australia will be diagnosed with breast cancer in their lifetime. Trans and gender diverse people can also be affected by breast cancer.
There are a range of factors that can influence your chance of developing breast cancer. These include both risk factors, which may increase your likelihood of developing breast cancer, and protective factors, which can help reduce risk. While not all breast cancers can be prevented, understanding these factors – and which can be modified – can support informed decisions about your health and wellbeing.
Read ahead for more information on breast cancer and risk factors.
How to minimise your risk of developing breast cancer
The incidence (number of new cases) of breast cancer is increasing over time. And while some risk factors – such as being a woman or person assigned female at birth, or getting older – cannot be changed, other risk factors can be changed or managed.
The following lifestyle factors have been linked to increased risk (or chance) of developing breast cancer. While some of these risk factors may increase the likelihood of developing breast cancer, having one or more of these risk factors does not mean that you will definitely develop breast cancer. Likewise, having no known risk factors also does not guarantee that you will never develop breast cancer. If you are concerned about any of these risk factors, see your doctor to discuss any concerns.
Modifiable lifestyle factors
Alcohol intake
According to Cancer Australia, it is estimated that approximately 6% of breast cancer cases each year in Australia are due to alcohol consumption.
Currently, there does not appear to be a ‘safe’ level of regular alcohol consumption for the risk of breast cancer. Drinking alcohol on a daily basis is associated with an increased risk of breast cancer in postmenopausal women and is likely to be associated with an increased risk of breast cancer in premenopausal women, too. The risk of breast cancer increases as the number of drinks regularly consumed increases.
Being overweight, obesity and weight gain
 For postmenopausal women, being overweight or obese, or gaining weight, is linked to an increased risk of breast cancer. Keeping to a healthy weight range reduces the risk of breast cancer. According to Cancer Australia, it is estimated that 8% of postmenopausal breast cancers each year in Australia are due to being overweight or obese.
For postmenopausal women, being overweight or obese, or gaining weight, is linked to an increased risk of breast cancer. Keeping to a healthy weight range reduces the risk of breast cancer. According to Cancer Australia, it is estimated that 8% of postmenopausal breast cancers each year in Australia are due to being overweight or obese.
Smoking
 There is evidence that suggests an association between smoking and increased breast cancer risk. Tobacco smoking may be associated with an increased risk of breast cancer for women who started smoking when they were younger or started smoking for many years before having their first child.
There is evidence that suggests an association between smoking and increased breast cancer risk. Tobacco smoking may be associated with an increased risk of breast cancer for women who started smoking when they were younger or started smoking for many years before having their first child.
Tobacco smoke also contains more than 70 chemicals that are known to cause cancer; smoking is known to cause several other cancers, including lung, throat, liver, bowel and bladder cancers.
Processed meats
Eating processed meat may be associated with an increased risk of breast cancer, particularly in postmenopausal women.
Physical activity
 Physical activity is associated with a reduced risk of breast cancer. Women of all ages who do large amounts of physical activity, including vigorous physical activity, have a decreased risk of breast cancer. According to Cancer Australia, it is estimated that nearly 8% of postmenopausal breast cancers in Australia each year are attributable to a lack of physical activity.
Physical activity is associated with a reduced risk of breast cancer. Women of all ages who do large amounts of physical activity, including vigorous physical activity, have a decreased risk of breast cancer. According to Cancer Australia, it is estimated that nearly 8% of postmenopausal breast cancers in Australia each year are attributable to a lack of physical activity.
Protective reproductive factors
Having children and breastfeeding
Isla’s Story
At just 34, Isla’s world was turned upside down with a breast cancer diagnosis while pregnant with her second child.
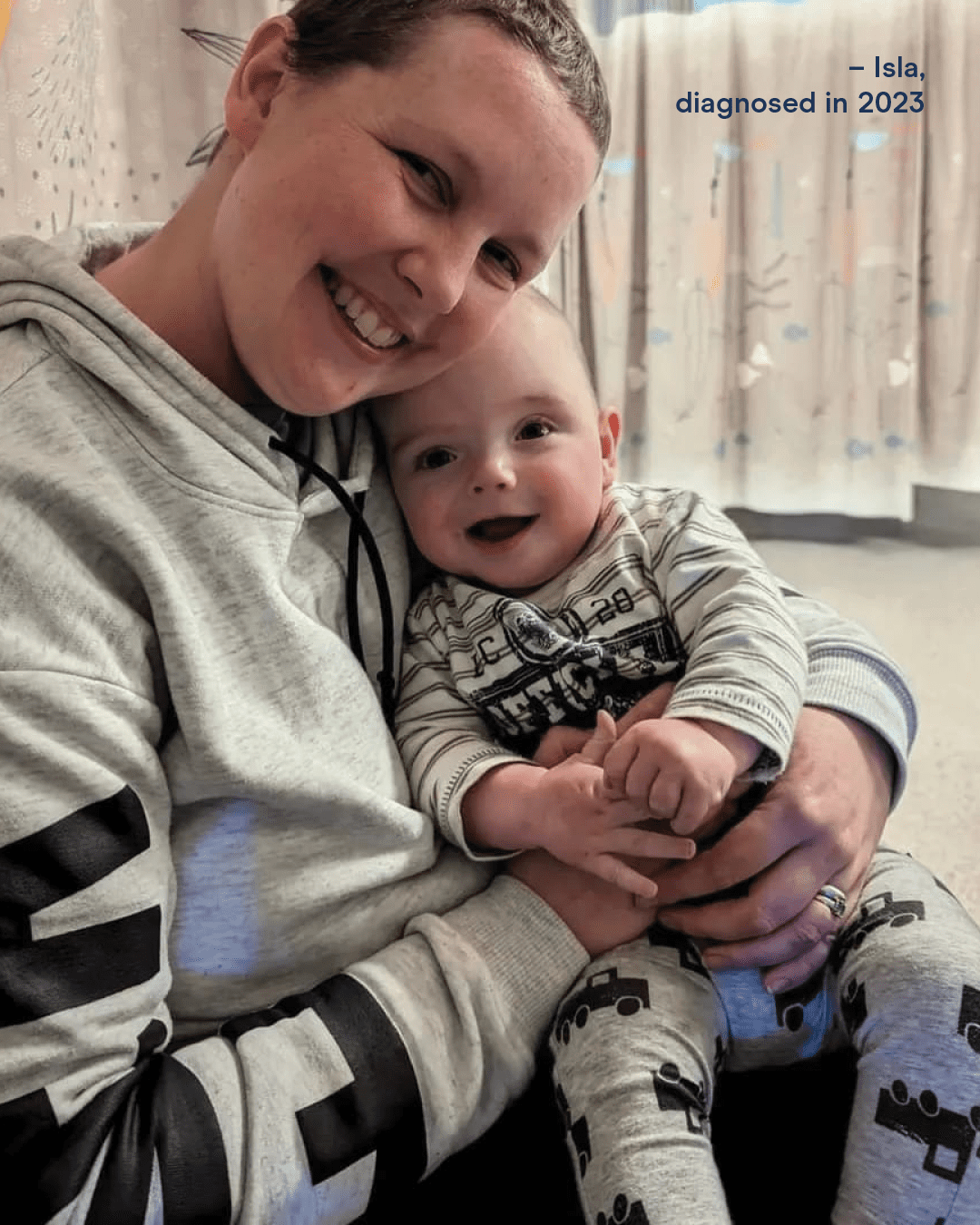
“Cancer can be a scary, overwhelming and a life-changing disease for so many. I want to be able to help others and say you are not alone in this journey. [I want to] raise awareness to get checked if something doesn’t feel right. I understand that not everyone will have the same journey and sadly not always a happy ending either, but I know that sharing experiences and positivity can make a world of difference.”
– Isla, diagnosed 2023
Thanks to research, Isla is now in remission – but her story is just one of the approximately 1,000 young women in Australia diagnosed with breast cancer each year.
Breast cancer risk factors you can’t change
While certain lifestyle factors can increase a person’s risk of developing breast cancer, many of these are modifiable and can be changed to help reduce that risk. However, there are also risk factors – such as age, sex assigned at birth and genetic predisposition – that cannot be changed (non-modifiable), which can increase your risk of being diagnosed with breast cancer. Understanding both types of risk factors is important for making informed decisions about your health.
Personal risk factors
Sex assigned at birth
 99% of breast cancer cases occur in women and people assigned female at birth. While some men do get breast cancer (estimated around one in 600), women are at a much higher risk (estimated at 1 in 7 women will be diagnosed).
99% of breast cancer cases occur in women and people assigned female at birth. While some men do get breast cancer (estimated around one in 600), women are at a much higher risk (estimated at 1 in 7 women will be diagnosed).
Ageing
 The older women get, the higher their risk of developing breast cancer. In Australia, breast cancer can occur in younger women, but about three out of four breast cancer cases occur in women aged 50 years and older. The average age of first diagnosis for breast cancer is 62 years.
The older women get, the higher their risk of developing breast cancer. In Australia, breast cancer can occur in younger women, but about three out of four breast cancer cases occur in women aged 50 years and older. The average age of first diagnosis for breast cancer is 62 years.
Birthweight and height
Having a higher birthweight is likely to be associated with an increased risk of breast cancer in premenopausal women. Cancer Australia estimates that the risk of premenopausal breast cancer increases by about 5% for each 500g increase in birthweight.
Being taller as an adult is also associated with an increased risk of breast cancer. Cancer Australia estimates that the risk of breast cancer increases by about 17% for each extra 10cm in a woman’s adult height.
Reproductive risk factors
Age when periods (or menstruation) started
 Starting periods at an early age (before the age of 12) is linked to a slightly increased risk of breast cancer. It is estimated that the risk of breast cancer increases by about 5% for each year younger women are when they begin menstruating.
Starting periods at an early age (before the age of 12) is linked to a slightly increased risk of breast cancer. It is estimated that the risk of breast cancer increases by about 5% for each year younger women are when they begin menstruating.
Late menopause
 Undergoing menopause later in life is linked to an increased risk of breast cancer. Menopause occurs when periods stop permanently. The average age of menopause for women in Australia is 51 years old. Women who reach menopause at 55 years old have about a 12% higher risk of breast cancer compared to those who reach menopause between 50-54 years old.
Undergoing menopause later in life is linked to an increased risk of breast cancer. Menopause occurs when periods stop permanently. The average age of menopause for women in Australia is 51 years old. Women who reach menopause at 55 years old have about a 12% higher risk of breast cancer compared to those who reach menopause between 50-54 years old.
Age when first child was born and not having children
Having a first child at an older age is associated with an increased risk of breast cancer. Research suggests that for each additional year older women are at the time of their first childbirth, the risk of developing breast cancer increases by approximately 3%.
Not having children is associated with a higher risk of developing breast cancer. Women who have never had children have approximately a 16% greater risk compared to those who have had at least one child.
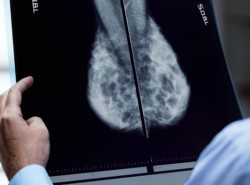
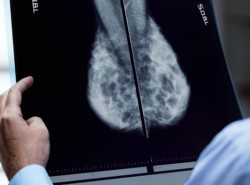
High breast density
 Having higher-than-average breast density, as detected through a mammogram, is associated with an increased risk of breast cancer. Breast density refers to the proportion of dense glandular tissue compared to fatty tissue in the breast. On a mammogram, dense tissue appears white, while fatty tissue appears dark. Breast density can only be measured by a mammogram and cannot be determined by how breasts look, feel, their size or firmness.
Having higher-than-average breast density, as detected through a mammogram, is associated with an increased risk of breast cancer. Breast density refers to the proportion of dense glandular tissue compared to fatty tissue in the breast. On a mammogram, dense tissue appears white, while fatty tissue appears dark. Breast density can only be measured by a mammogram and cannot be determined by how breasts look, feel, their size or firmness.
Family history and genetics
Family history
 A family history of breast cancer means having one or more first-degree or second-degree relatives who have been diagnosed with breast cancer. The relative can be from either side of the family.
A family history of breast cancer means having one or more first-degree or second-degree relatives who have been diagnosed with breast cancer. The relative can be from either side of the family.
The significance of family history increases with the number of affected family members and the age they were diagnosed. For example, your breast cancer risk is increased if you have a strong family history, such as three or more first or second-degree relatives on the same side of the family with breast or ovarian cancer, especially if they were diagnosed with cancer at a young age.
Some women may inherit a specific genetic variation (or mutation in a gene) that increases the risk of breast cancer. Only about 5-10% of breast cancer cases can be explained by an inherited mutation.
BRCA1 and BRCA2 genes
 Having a fault (or mutation) in the BRCA1 and BRCA2 genes is associated with an increased risk of breast and ovarian cancer. BRCA1 and BRCA2 mutations are considered rare. About 1 in 400 to 1 in 800 people have a BRCA1 or BRCA2 gene mutation. Over their lifetime, women who carry a mutation in one of these genes have about a 70% chance of developing breast cancer. However, not everyone who has a faulty BRCA1 or BRCA2 gene will develop cancer.
Having a fault (or mutation) in the BRCA1 and BRCA2 genes is associated with an increased risk of breast and ovarian cancer. BRCA1 and BRCA2 mutations are considered rare. About 1 in 400 to 1 in 800 people have a BRCA1 or BRCA2 gene mutation. Over their lifetime, women who carry a mutation in one of these genes have about a 70% chance of developing breast cancer. However, not everyone who has a faulty BRCA1 or BRCA2 gene will develop cancer.
If you are concerned that you may have an increased risk of breast cancer, please speak with your GP or local family cancer clinic, who will help you assess your risk and refer you for further genetic testing if needed.
Hear from Associate Professor Juliet French on research into breast cancer genetic factors
iPrevent
 To help Australians know and manage their personal breast cancer risk, NBCF has funded the innovative work of Professor Kelly-Anne Phillips. Her development of web-based tool, iPrevent, was designed help Australian women to estimate their risk of developing breast cancer so they can take appropriate action.
To help Australians know and manage their personal breast cancer risk, NBCF has funded the innovative work of Professor Kelly-Anne Phillips. Her development of web-based tool, iPrevent, was designed help Australian women to estimate their risk of developing breast cancer so they can take appropriate action.
Last updated: November 2025
Frequently Asked Questions about breast cancer prevention and risk
The evidence that phytoestrogens (plant oestrogens) and soy products in the diet are associated with breast cancer risk is inconclusive. Only a small number of studies have been performed and the evidence is inconsistent; however, analyses of higher quality cohort studies show no association with breast cancer risk for intake of any specific group of dietary oestrogens, including ‘isoflavones’ (a type of phytoestrogen found in soybeans and soy products) and soy and soy products.
There are a range of factors that contribute to your chance of developing breast cancer. Some risks can be reduced (such as limiting alcohol), while others you might have no control over (such as genetics). Although some factors may increase your risk of developing breast cancer, having one or more of these risk factors does not mean that you will definitely develop cancer. Likewise, having no known risk factors also does not guarantee that you will never develop cancer. It is recommended that you speak to your doctor if you are worried about your risk of developing breast cancer.
There is no conclusive evidence that silicone-filled breast implants are associated with risk of breast cancer. Several studies have been done, and while these have had limitations, none has conclusively shown any link between silicone breast implants and increased risk of breast cancer.
Related Research
 Having children is a protective factor that is linked to a reduced risk of breast cancer. According to Cancer Australia, the risk of breast cancer decreases by 7% for each child the women has had. Breastfeeding is likely to be associated with a small decreased risk of breast cancer as well – the longer the duration of breastfeeding, the lower the risk of breast cancer.
Having children is a protective factor that is linked to a reduced risk of breast cancer. According to Cancer Australia, the risk of breast cancer decreases by 7% for each child the women has had. Breastfeeding is likely to be associated with a small decreased risk of breast cancer as well – the longer the duration of breastfeeding, the lower the risk of breast cancer.