Around 1,000 young women are diagnosed with breast cancer every year in Australia.
Contents
- Breast cancer in young women
- Martine’s story: Diagnosed at 29 years old
- Common breast cancer issues affecting young women
- Breast cancer risk factors for young women
- Detection and diagnosis of breast cancer in young women
- NBCF-funded research on breast cancer in young women
- Frequently Asked Questions about breast cancer in young women
Breast cancer in young women
Each year, around 1,000 young women aged under the age of 40 will be diagnosed with breast cancer in Australia, and 69 are estimated to die from this disease. That’s about three young women diagnosed every day and about one young woman dying each week from breast cancer.
Around 80% of women diagnosed with breast cancer are over 50 years old. While there are many more older women being diagnosed with breast cancer, it is the most commonly diagnosed cancer in younger women under 40. Sadly, it is also the leading cause of death from cancer in this age group.
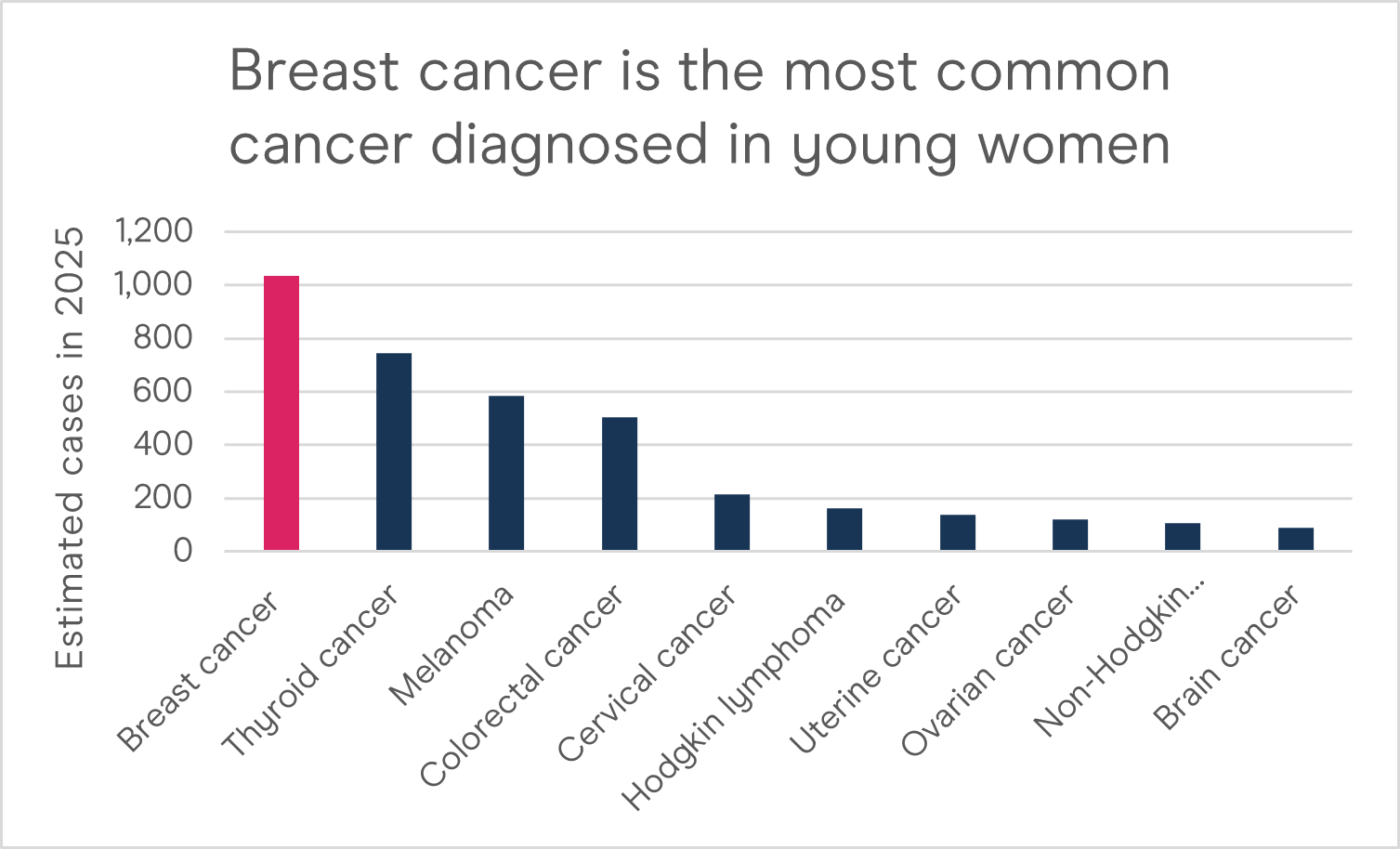
Breast cancer is the most common cancer diagnosed in young women in Australia. Source: Australian Institute of Health and Welfare. (2025). Cancer data in Australia.
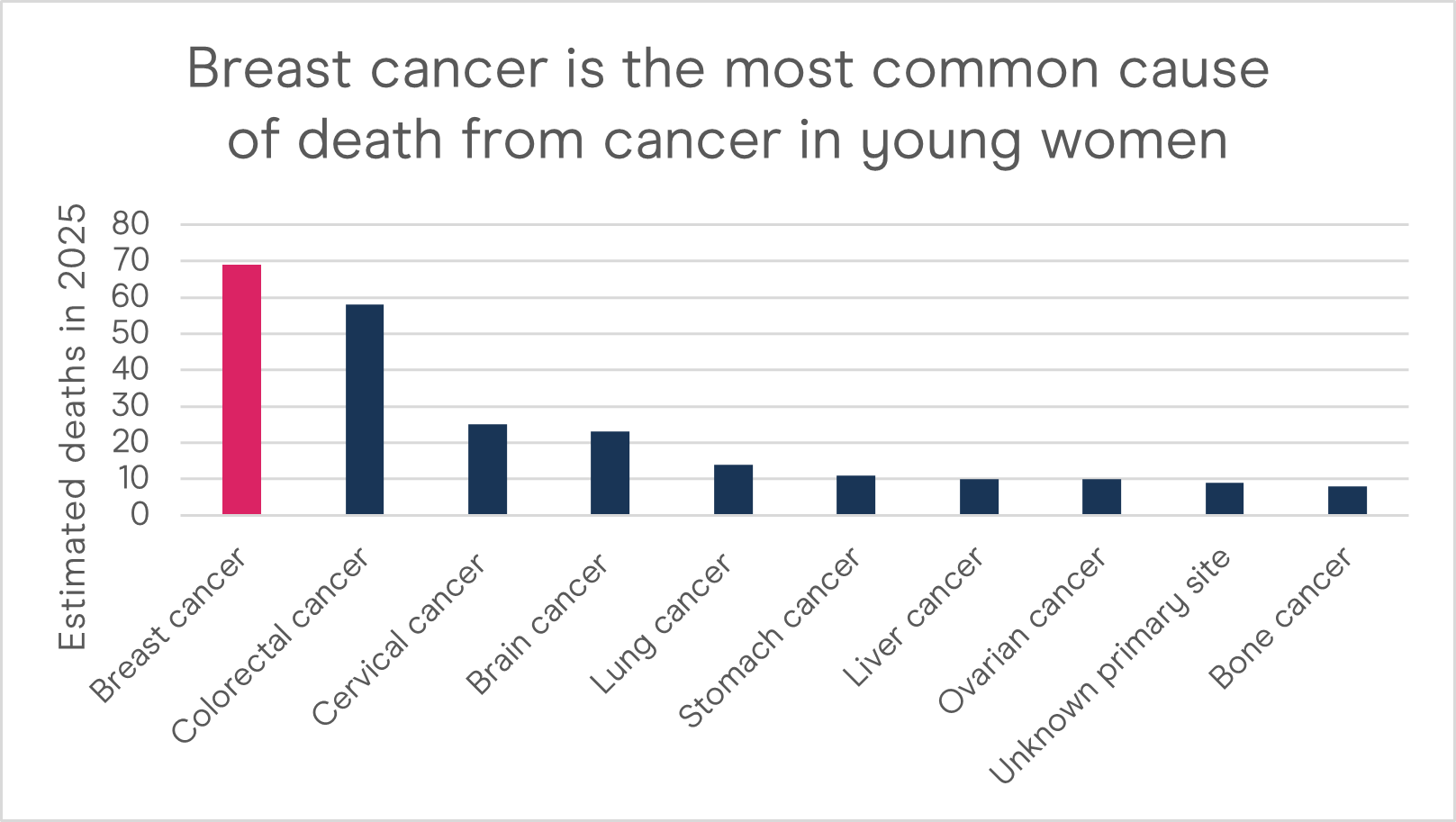
Breast cancer is the most common cause of death from cancer in young women. Source: Australian Institute of Health and Welfare. (2025). Cancer data in Australia.
According to Cancer Australia, almost 20% of young women living with breast cancer are diagnosed at a locally advanced stage (stage 3). Young women are also more likely to be diagnosed with more aggressive breast cancers like Triple Negative Breast Cancer (TNBC).
Between 1982–2025 in Australia:
- The number of new cases of breast cancer diagnosed in women aged 20–39 increased from 502 to 1,035.
- The age-specific incidence rate of breast cancer increased by around 24% from 21 cases per 100,000 females to 26 cases per 100,000 females.
Between 1982–2025 in Australia:
- The number of deaths from breast cancer in women aged 20–39 decreased from 101 to 69 deaths.
- The age-specific mortality rate of breast cancer decreased by around 64% from 4.2 deaths per 100,000 females to 1.7 deaths per 100,000 females.
Martine’s story: Diagnosed with breast cancer at 29 years old
Martine was diagnosed with breast cancer at just 29 years old after finding two lumps during her routine breast self-exam. For young women, it is vital to be breast aware and know how their breasts look and feel.
Within three weeks, Martine had a mastectomy with reconstruction and went through fertility treatment, port insertion, five months of chemotherapy and six weeks of radiotherapy.
Common breast cancer issues affecting young women
While breast cancer in women under 40 is relatively uncommon, the impact of the disease can be devastating. Young women face a unique set of practical, physical and psychosocial challenges.
Receiving a diagnosis of breast cancer at any age can be a shock. Younger women often report feeling socially isolated or alone during and after breast cancer treatment – even if they are surrounded by supportive family and friends. A diagnosis of breast cancer may also impact a young woman’s career and financial situation.
There are supportive resources available for young women affected by breast cancer. Breast Cancer Network Australia (BCNA) offers resources that provide emotional and practical support for people affected by cancer, including information tailored to young women, personal stories about young women living with breast cancer, a peer-to-peer Online Network, and a confidential Helpline (1800 500 258). BCNA also provides advice on employment and support with discrimination.
Physical burden of breast cancer
Breast cancer treatments may cause physical side effects such as fatigue, sleep problems, weight gain, issues with cardiovascular health, and reduced bone mineral density, which increases the risk of early-onset osteoporosis and osteopenia in young women. Notably, breast cancer can also have an impact on fertility.
Impact of breast cancer treatment on fertility and pregnancy
Many young women diagnosed with breast cancer are concerned about fertility. Treatments for breast cancer may affect fertility temporarily or permanently as they can cause early menopause, known as medically induced menopause, and associated symptoms.
The impact of breast cancer treatments like chemotherapy and radiation therapy (radiotherapy) on fertility depends on a number of factors. These include age and the type, dose and duration of treatment received. Side effects of treatment can also vary among different women of the same age.
Treatments for breast cancer may have a temporary or permanent impact on fertility as they can cause medically induced menopause. The physical changes related to breast cancer itself and side effects of treatment may also have an impact on body image, sense of sexual wellbeing, and intimate relationships. Breast Cancer Network Australia (BCNA) has further resources on breast cancer and sexual wellbeing, as well as booklets and fact sheets to support women facing breast cancer.
Psychological burden of breast cancer
Physical changes to the body caused by breast cancer treatment may also have a significant effect on sexuality, intimacy, self-image, self-esteem, and mental and emotional wellbeing. Breast cancer treatments can involve a mastectomy, and other treatments can lead to side effects such as medically induced menopause, hair loss, changes to the vagina, loss of libido and weight gain. These physical changes can further cause psychological distress, loss of confidence and negative feelings.
Fear of recurrence is the fear that breast cancer could return in the breast/s or in another part of the body. Even following treatment from breast cancer, many people of all ages live with an ongoing fear that their cancer will return. Unfortunately, 15% of people will experience a recurrence within 10 years, and young people (particularly those under 35) may face an increased risk of recurrence.
The fear of breast cancer recurrence can be debilitating, leading to anxiety, depression and reduced quality of life. Visiting BCNA’s Online Network or contacting BCNA’s confidential Helpline on 1800 500 258 may be useful for those experiencing fear of breast cancer recurrence.
Breast cancer risk factors for young women
All women are at risk of developing breast cancer and the risk greatly increases with age.
There are a range of factors that can increase breast cancer risk. According to Cancer Australia, young women may have an increased risk of breast cancer due to factors such as:
- Family history – The risk of breast cancer is increased if you have a strong family history, such as three or more first or second-degree relatives on the same side of the family with breast or ovarian cancer, and if any relatives were diagnosed with cancer at a young age.
- Genetic susceptibility – This accounts for up to 10% of breast cancers in young women. Such genetic factors include inherited mutations in BRCA1 or BRCA2 genes (or gene mutations).
- Reproductive and hormonal factors – Early menarche (age at first period) and late menopause increase the risk of breast cancer.
What reduces breast cancer risk?
- Keep your alcohol consumption down – Drinking alcohol can increase the risk of breast cancer for people of all ages. Currently, there does not appear to be a ‘safe’ level of regular alcohol consumption for the risk of breast cancer.
- Physical activity – Women of all ages who engage in physical activity are at reduced risk of breast cancer compared to women who do not exercise.
- Childbearing and breast feeding – Having children at a younger age is associated with a decreased risk of breast cancer. The more children women have, the more their risk of breast cancer appears to be reduced. Breastfeeding can also reduce breast cancer risk.
If you are concerned that you may have an increased risk of breast cancer, please speak with your GP or local family cancer clinic.
If you are classified as being at high-risk of developing breast cancer, particularly if you have a family history and mutations in the BRCA1 and BRCA2 genes, you should discuss an individual routine screening program with your GP.
Detection and diagnosis of breast cancer in young women
Breast cancer screening aims to detect breast cancer at an early stage, when it is more treatable. In Australia, BreastScreen Australia is a population-based screening initiative that offers women over 40 free mammograms (an x-ray of the breast) every two years. This program is also inclusive of trans and gender diverse people. There is currently insufficient evidence that mammography is an effective breast cancer screening strategy for women under 40.
People of all ages should be aware of how their breasts normally look and feel, and report any new or unusual changes to their GP without delay.
See here for breast cancer symptoms
NBCF-funded research on breast cancer in young women
The National Breast Cancer Foundation (NBCF) has funded several research projects related to breast cancer in young women over the years. These projects cover a broad research spectrum, including:
- Identifying genetic risk factors and new treatments for young people affected by breast cancer
- Working towards a prevention strategy for individuals with a faulty BRCA2 gene
Most recently, NBCF invested $25 million over five years into a pioneering research program called AllClear through our first-ever Collaborative Research Accelerator Grant. AllClear aims to understand why and how cancer recurs, and find ways to detect and eliminate dormant cancer cells that have spread to the bone – before they ‘reawaken’ and cause metastatic disease. This research could benefit younger women affected by breast cancer, who may face a higher risk of recurrence and live with the ongoing fear that their cancer could return someday.
Last updated: January 2026 (using 2025 AIHW cancer data)
Frequently Asked Questions about breast cancer in young women
People of all ages can be diagnosed with breast cancer. While it is more common in women aged 50 or older, around 1,000 women under 40 are still diagnosed with breast cancer in Australia each year.
It is important for people of all ages to be breast aware and know the feel and look of their breasts, so any new or unusual changes that may indicate breast cancer can be detected.
Common changes that could be due to breast cancer include:
- a lump or thickening in the breast, especially if it’s only in one breast
- a change in the shape or size of the breast or nipple
- dimpling of the skin or the nipple
- discharge or blood from the nipple
- a rash or changes to the skin around the breast
- persistent pain in the breast or armpit
- swelling or a lump in the armpit
While most changes to the breast may not be due to breast cancer, you should visit your GP immediately if you notice anything new or unusual. Your GP may then do a clinical breast exam and order imaging such as an ultrasound.
If you are under 40, you may be at increased risk if you have a strong family history of breast cancer, such as three or more first or second-degree relatives on the same side of the family with breast or ovarian cancer, and any relatives diagnosed with cancer at a young age. Having inherited genetic mutations such as BRCA1 or BRCA2 can also predispose you to breast cancer at an earlier age. You can learn more about genetic mutations related to breast cancer here.
While there is no definitive way to prevent breast cancer, there are still ways to manage and reduce your breast cancer risk by focusing on lifestyle-based factors that you can modify, such as your alcohol consumption, being overweight and obesity after menopause, level of physical activity, and tobacco use (smoking).
BCNA offers resources that provide emotional and practical support for people affected by cancer, including young women. You can also access BCNA’s peer-to-peer Online Network and confidential Helpline on 1800 500 258.
